In recent years, the field of gut microbiome has seen a notable increase in interest in medical research, motivated by new insights into the potential impact of gut microbiota on several organ systems, particularly offering beneficial effects on the brain. The cognitive functions related to overall wellbeing, learning and memory, and the connection of the use of probiotics and prebiotics have been discussed in research (Bhandari & Vlas, 2025). However, this topic remains underrepresented in nursing education.
![[Alt-text: Woman holding a flower on her stomach, with her hands forming a heart shape around it.]](https://blogit.lab.fi/labfocus/wp-content/uploads/sites/8/2025/06/233_2025_From-the-gut-to-the-bedside-integrating-microbiome-knowledge-in-the-nursing-education_1-1024x583.jpg)
Microbiota and probiotics: linking gut health to overall wellbeing?
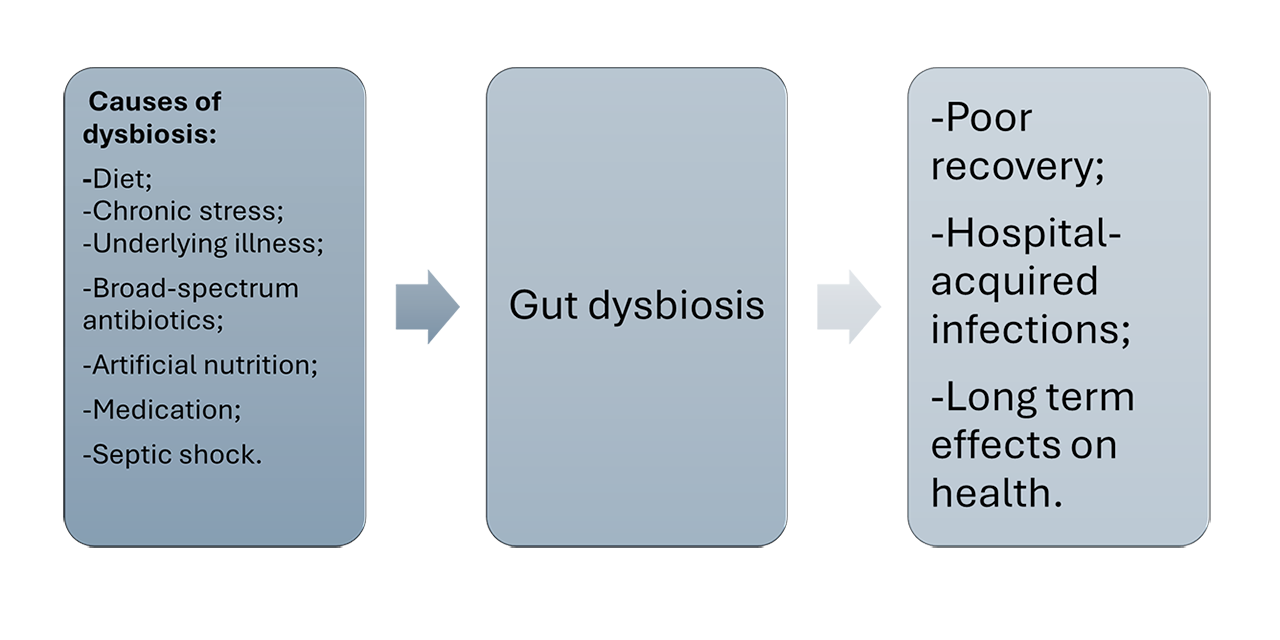
The composition of the gut microbiota is mostly dominated by bacteria. The bacterial community is individually adapted, and it is undergoing evolution throughout the lifespan. This evolution is influenced by various factors, including stress, environment, diet, medication, and aging. The symbiotic relationship between beneficial bacteria and the gastrointestinal tract has been shown to have numerous positive effects on overall health. However, an increase in the population of harmful bacteria can disrupt the balance of the microbiome, inducing a state of dysbiosis. (Wiertsema et al. 2021.)
Chronic stress has been identified as a key factor in the development of gut dysbiosis. The phenomenon of gut dysbiosis has been shown to cause gut permeability, allowing bacteria to penetrate the bloodstream and cross the brain-blood barrier. Several studies show that it has resulted in elevated levels of inflammation within the body and the brain tissue. This can consequently lead to the premature aging of the brain. (Alsegiani et al. 2022; Nandwana et al. 2022.; Bhandari & Vlas 2025.)
Hospitalization and the changes in the gut microbiota
The overgrowth of certain bacterial species may serve as an indicator of potential gut dysfunction. A recent study investigated the alterations in the composition of the gut microbiota and the bedside treatment of critically ill patients. The findings indicated a significant change in the microbiota composition of the patients from the onset of their hospitalization.
The underlying cause of this deterioration in the gut was linked to several factors, including the underlying illness, the administration of broad-spectrum antibiotics, the use of artificial nutrition, the medication affecting GI tract, or sepsis. These factors have a negative impact on the diversity of beneficial bacteria, therefore creating an environment favorable for the overgrowth of multidrug-resistant organisms. This, in turn, has been shown to increase the incidence of hospital-acquired infections and can increase mortality. (Szychowiak et al. 2022.) This finding indicates that understanding the dynamics of gut microbiota is essential for predicting disease progression and mitigating the long-term consequences of bedside treatment.
The need for awareness in nursing education
The integration of evidence from the field of microbiome research into the nursing curriculum has the potential to enhance patient care. Bhandari and Vlas (2025) state that the research done on human microbiota is lacking, with many studies in this area coming from animal models. The primary focus of new potential research should be on the early detection of gut dysbiosis. This could be achieved through the individual analysis of the gut microbiota composition and continuous monitoring in healthcare settings.
Additionally, dietary interventions, such as prebiotic and probiotic supplementation, could be included as complementary strategies to preserve microbial diversity and can be beneficial to specific patient groups. Health care professionals could pay more attention to the effects of gut health and therefore the topic should be better addressed in the nursing curricula and continuous education of graduated professionals. (Bhandari & Vlas 2025.)
Authors
Ariana Vlas is a graduate paramedic nursing student at LAB University of Applied Sciences.
Sini Hämäläinen works as a Senior Lecturer at LAB University of Applied Sciences.
References
Alsegiani, A.S. & Shah, Z.A. 2022. The influence of gut microbiota alteration on age-related neuroinflammation and cognitive decline. Neural Regeneration Research. Cited 19 May 2025. Available at https://doi.org/10.4103/1673-5374.335837
Bhandari S. & Vlas A. 2025. Improving cognitive functions with prebiotics and probiotics and discussing their relation to gut health – A nursing perspective. Cited 19 May 2025. Available at https://urn.fi/URN:NBN:fi:amk-2025051512040
Nandwana, V., Nandwana, N.K., Das, Y., Saito, M., Panda, T., Das, S., Almaguel, F., Hosmane, N.S. & Das, B.C. 2022. The role of microbiome in brain development and neurodegenerative diseases. Molecules. Vol. 27, 3402. Cited 18 May 2025. Available at https://doi.org/10.3390/molecules27113402
silviarita. 2018. Nainen, vatsa, vatsakipu, sydän. Pixabay. Cited 9 June 2025. Available at https://pixabay.com/fi/photos/nainen-vatsa-vatsakipu-syd%C3%A4n-3186730/
Szychowiak, P., Villageois-Tran, K., Patrier, J., Timsit J.-F., Ruppé, E. 2022. The role of the microbiota in the management of intensive care patients. Ann. Intensive Care. Cited 19 May 2025. Available at https://doi.org/10.1186/s13613-021-00976-5
Wiertsema, S.P., van Bergenhenegouwen, J., Garssen, J. & Knippels, L.M.J. 2021. The interplay between the gut microbiome and the immune system in the context of infectious diseases throughout life and the role of nutrition in optimizing treatment strategies. Nutrients. Vol. 13(3), 886. Cited 19 May 2025. Available at https://doi.org/10.3390/nu13030886